Cartilage Damage in the Knee
Causes
Cartilage damage in the knee occurs either due to wear and tear or an accident.
A special form is OCD – Osteochondritis dissecans, which has a staged progression and can arise spontaneously, among other things. This involves a gradual death of cartilage tissue due to undersupply and/or overuse.
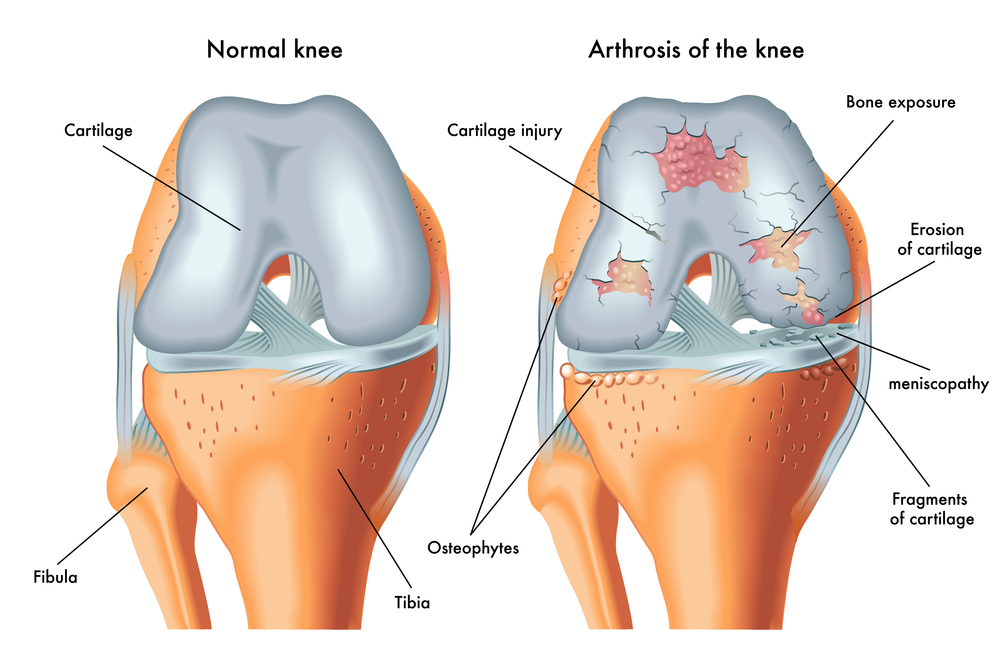
If there is damage to the cartilage, it has a very poor tendency for spontaneous healing, which usually leads to an increase in the extent of the damage and worsening symptoms over time. Isolated cartilage damage can enlarge, gradually leading to the development of osteoarthritis. Cartilage damage can promote the formation of a Baker’s cyst.
Localization of Cartilage Damage in the Knee
Common locations for cartilage damage are the inner and outer sides of the femoral condyles, which are subjected to asymmetrical stress depending on the leg axis (knock-knees or bow-legs). Cartilage damage can also be located in the patellofemoral joint, which can be damaged either by chronic overuse or traumatically, e.g., after a patellar dislocation.
Diagnosis of Cartilage Damage in the Knee
The diagnosis is primarily made clinically (pain) and by plain radiography (X-ray). A magnetic resonance imaging (with cartilage-specific sequences) is absolutely necessary.
Treatment of Cartilage Damage
Smaller cartilage defects can in most cases be treated without surgery. Larger defects require surgery.
Conservative Treatment
Conservatively, cartilage damage can be treated with hyaluronic acid injections and relieving measures, as well as in special cases with infusion therapies .
Surgery
Surgically, there are several options for cartilage damage in the knee. The appropriate procedure must be decided depending on the extent, nature, and location.
Minced Cartilage – Regenerative Cartilage Therapy
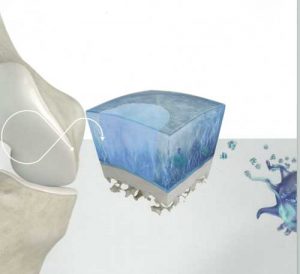 Minced cartilage is a novel therapy to surgically fill cartilage defects in a joint. In a single minimally invasive operation, autologous cartilage is processed and used to fill the defect. The procedure can be performed as part of an arthroscopy, i.e., through 2.5mm small skin incisions.
Minced cartilage is a novel therapy to surgically fill cartilage defects in a joint. In a single minimally invasive operation, autologous cartilage is processed and used to fill the defect. The procedure can be performed as part of an arthroscopy, i.e., through 2.5mm small skin incisions.
Once sufficient donor cartilage has been harvested, the preparation process begins:
Autologous blood is drawn and specially processed. This yields growth factors on the one hand, and the ‘glue’ of the blood on the other. The cartilage graft is prepared with the autologous blood. The cartilage fragments are mixed with the ‘blood glue’ to form a paste, which is then introduced into the cartilage defect and fills it. To give the graft even more stability, it is dabbed with growth factors and blood glue and fixed.
Fragment Refixation
Sheared-off larger cartilage fragments can be fixed with screws or pins.
Microfracture
By drilling into the exposed bone, stem cells reach the surface and form a blood clot. From this, a substitute fibrocartilage can form. The procedure can be performed arthroscopically.
Mosaicplasty (OATS = osteochondral autologous transplantation)
In this method, the defective cartilage area is removed with a cylindrical punch and replaced with a cartilage-bone cylinder of appropriate size. This is taken from a peripheral area of the cartilage lining that is minimally stressed and needed. Alternatively, an artificial cartilage cylinder can be chosen – BioCartilage. The procedure can be performed arthroscopically.
Autologous Chondrocyte Implantation (ACI)
To be able to transplant cartilage, a biopsy is taken in a first arthroscopic procedure, from which autologous cartilage is cultivated over a period of approx. 6 weeks. This is then implanted into the cartilage defect in a second operation.
Postoperative Care for Cartilage Damage in the Knee
Postoperatively, the joint must be immobilized and relieved of stress.

Dr. Mark Schurz
CONTACT